EMS Training Bulletin 15-001 Accidental Hypothermia
Purpose:
1. To provide patient assessment and management guidance to UTSW/BioTel EMS Providers about Accidental Hypothermia
Background and Definition:
- Definition: an involuntary drop in core (internal) body temperature to 35°C (95°F) or less
- Primary: excessive cold overcomes heat production in an otherwise healthy person
- Secondary: caused by many medical conditions*, even in a warm environment
- Resuscitation outcomes can be favorable in many cases, even after prolonged “down time”
- Death in secondary hypothermia is often caused by the underlying condition
- Patient care goals: maintain hemodynamic stability, prevent further heat loss, aggressively resuscitate cardiac arrest and prevent limb loss (due to associated local cold injury)
Diagnosis and Clinical Features:
- Diagnostic Criteria:
- History of cold exposure OR a predisposing disease/risk factor* AND
- Cold torso OR core (internal) temperature less than 35°C (95°F)
- Core temperature cannot be measured by EMS, so use this clinical staging table:
| Table 1 – Clinical Staging of Accidental Hypothermia† |
| Stage |
Torso + These Signs and Symptoms |
Typical Core Temperature |
| I |
Conscious, shivering |
35 to 32°C (95 to 90°F) |
| II |
Impaired consciousness, not shivering |
Less than 32 to 28°C
(Less than 90 to 82°F) |
| III |
Unconscious, not shivering, vital signs present |
Less than 28 to 24°C
(Less than 82 to 75°F) |
| IV |
No vital signs, fixed and dilated pupils |
Less than 24°C
(Less than 75°F) |
†Adapted from Brown DJA, et al. 2012. NEJM 367:20; 1930-1938.
*Refer to the Table of Secondary Conditions (Table 3) below
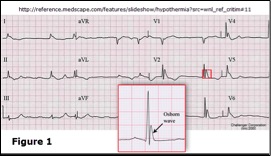
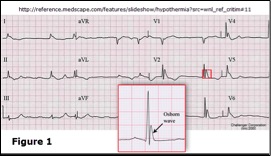
- ECG Findings – Slow cardiac conduction causes a range of dysrhythmias, such as:
- Sinus bradycardia and AV nodal block – generally resolve with rewarming
- Atrial fibrillation: common at core temperature less than 32°C (90°F)
- Osborn (J) waves: 80% of patients with core temperature less than 30°C (86°F)
- Late, small wave after the QRS in leads II, III, aVR, aVF & V3-V6 (Figure 1):
- Cardiac arrest: greatest risk in Stage III (core temperature less than 28°C (82°F))
- “Rescue Collapse”:
- Causes: Hypovolemia, dysrhythmias triggered by patient movement (ventricular fibrillation leading to asystole) and continued cooling
Pre-Hospital Patient Care and Transport:
- NOTE: Careful handling – minimize patient movements
- Patients in Stage II or III should NOT be permitted to stand, ambulate or exercise, in order to reduce risk of cardiac dysrhythmias and circulatory collapse
- NOTE: Detection of palpable pulse is difficult – check for signs of life/pulse for at least 60 seconds
- General Principles:
- Apply continuous ECG, SpO2 and ETCO2 monitoring
- Obtain and document frequent vital signs, including GCS and POC Glucose:
- Treat hypoglycemia per ALTERED LOC Treatment Guidelines
- Document the patient’s initial temperature and the ambient temperature (if known):
- Do not interrupt or delay treatment or transport for repeat measurements
- Core cooling may continue after rescue, once peripheral, active, external rewarming of cold extremities has begun – this is called “Afterdrop”
- Apply supplemental oxygen (warmed, if possible) to maintain SpO2 at least 94%
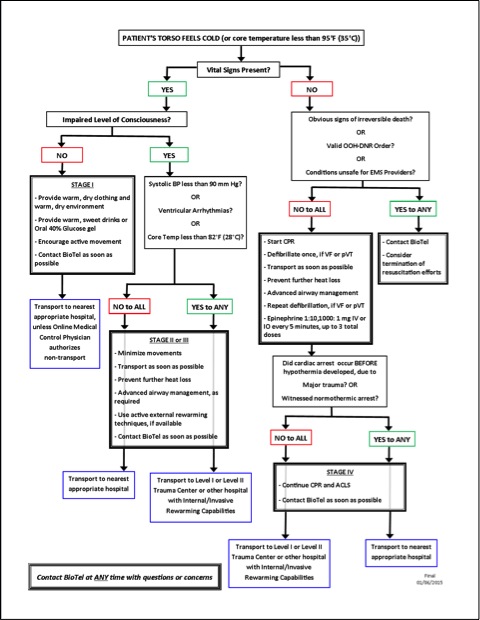
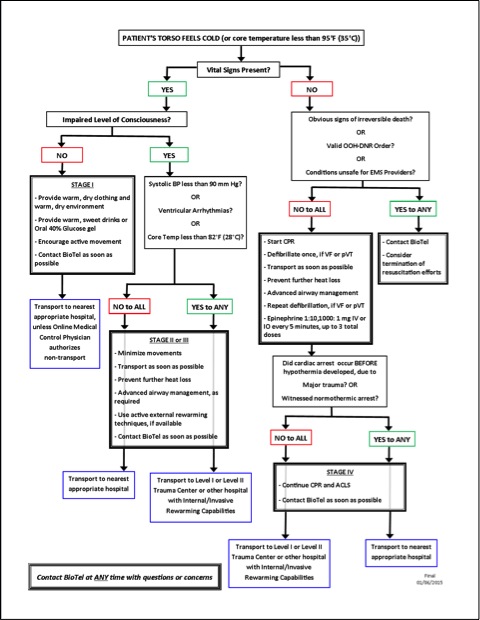
- Treat only hemodynamically significant dysrhythmias (e.g. ventricular fibrillation and pulseless ventricular tachycardia) and cardiac arrest – Refer to Figure 2 (page 3):
- Sinus bradycardia: consider pacing ONLY if hemodynamic compromise persists after rewarming
- VF/pVT: up to 3 defibrillation attempts & 3 doses of epinephrine, as needed
- Establish IV/IO access, but avoid excessive infusions of cold fluids
- Treat associated and underlying condition(s) (Table 3, page 5), including Cardiac Arrest, per standard UTSW/BioTel EMS Treatment Guidelines
- Pre-Hospital Patient Care and Transport Overview (Figure 2):
- Methods for Passive Rewarming and Prevention of Further Heat Loss:
| Table 2 – Rewarming Methods for Accidental Hypothermia |
| Pre-Hospital |
Hospital |
| Passive |
Active – External |
| Dry Patient |
Heating Pad, Warm Water Bottles |
| Shelter from wind and wet conditions, insulate from ground |
Immersion in Warm Bath |
| Move patient to warm environment |
External Convection Heaters (e.g. Lamps) |
| Blanket or Clothing Insulation |
Forced Air Warming Blankets (Bair Hugger®) |
| Head Cover |
Active – Internal (See Appendix) |
| Heat Packs, Warm Water Bottles, if available |
Catheter, Body Cavity Lavage, Peritoneal Dialysis |
| Shivering: increases heat production, but requires caloric replacement (if possible) |
Extracorporeal Rewarming (See Appendix) |
| Provide warm, sweet drinks or 40% oral glucose gel to alert patients with normal airway |
ECMO, Cardiopulmonary Bypass, Hemodialysis |
- Special Considerations:
- Contraindications for initiating resuscitation in the hypothermic patient:
- Submersion greater than 1 hour
- Core temperature less than 10°C (50°F)
- Obvious fatal injuries, such as decapitation
- Ice formation in the airway and other signs of total body tissue freezing
- Chest wall rigidity that renders chest compressions impossible
- Valid Out-of-Hospital DNR Order
- Dangers to EMS Providers or other rescuers
- Additive Effect of Major Trauma:
- Trauma, shock and cerebrospinal injury increase risk of hypothermia
- Hypothermia increases bleeding, transfusion requirement and mortality
- Refer to the TRAUMA Treatment Guidelines
- Submersion/Drowning:
- Cold water submersion: outcome may be more favorable than warm water
- Continue resuscitation if submersion time is less than 60 minutes or unknown and there are no contraindications to resuscitation (Section 6a, above)
- Associated Local Cold Injury, e.g. Frostbite:
- Remove clothing, footwear, jewelry and other constricting items
- Initiate rewarming, if feasible, ONLY if refreezing is absolutely preventable
- Do not allow tissue to refreeze!
- Cover injured parts with a loose, dry sterile dressing
- Do not open or drain intact blisters
- Do not rub the injured part to stimulate circulation
- Maintain affected body part at heart level:
- Do not elevate or allow limb to dangle
- Refer to the PAIN MANAGEMENT Treatment Guidelines
Destination Decision-Making – Consult BioTel or Hospital Capabilities Matrix:
- Stage I (Conscious, shivering and no other signs/symptoms): Nearest appropriate hospital, unless the Online Medical Control Physician advises otherwise
- Stage II (Impaired consciousness or not shivering):
- Normal BP, no dysrhythmia and core temp at least 28°C (82°F): Nearest appropriate hospital
- Hypotension or dysrhythmia or core temp less than 28°C (82°F): Level I or Level II Trauma Center, or a hospital capable of internal/invasive rewarming
- Stage III (Unconscious, not shivering and vital signs present): Level I or Level II Trauma Center, or a hospital capable of internal/invasive rewarming
- Stage IV (Absent vital signs, CPR): Level I or Level II Trauma Center, or a hospital capable of internal/invasive rewarming
- Exception: nearest appropriate hospital IF cardiac arrest occurred before hypothermia developed, e.g. due to trauma or witnessed normothermic arrest
Critical Documentation Items:
- Duration of cold exposure, ambient temperature at time of EMS contact, and rewarming attempts or other therapies performed prior to EMS arrival
- Cardiac dysrhythmias and treatment and associated trauma (when present)
| Table 3 – Examples of Conditions Associated with Secondary Hypothermia† |
| Impaired Thermoregulation |
Increased Heat Loss |
| Central Nervous System Disease, e.g. Stroke |
Multi-System Trauma |
| Central Nervous System Trauma |
Shock |
| Spinal Cord Transection |
Burns |
| Extremes of age: Newly Born and Elderly |
Cardiopulmonary Disease |
| Alcoholic or Diabetic Ketoacidosis |
Major Infection (bacterial or viral or parasitic) |
| Lactic Acidosis |
Emergency Childbirth |
| Hypoglycemia |
Cold IV or IO Infusions |
| Extreme Physical Exertion |
Heat-Stroke Treatment |
| Malnutrition |
Disseminated Cancer |
| Hypothyroidism and Other Endocrine Diseases |
Medication- and Toxin-Induced Skin Diseases |
| Impaired Shivering |
|
†Adapted from Brown DJA et al. 2012. NEJM 367:20; 1930-1938.
Summary:
- EMS Providers must screen for accidental hypothermia, even in a relatively warm environment, especially in patients with a wide range of conditions and diseases (Table 3)
- Patient care goals: maintain hemodynamic stability, prevent further heat loss, aggressively resuscitate cardiac arrest and prevent limb loss
- Patients with Stage I hypothermia should be transported to the nearest appropriate facility, unless the Online Medical Control Physician advises otherwise
- Most patients with Stage II and III hypothermia should be transported to a Level I or Level II Trauma Center, or to a hospital capable of internal/invasive rewarming procedures (Consult the Hospital Capabilities Matrix or BioTel for destination assistance)
- For patients with Stage IV hypothermia and cardiac arrest/CPR due to ventricular fibrillation (VF) or pulseless ventricular tachycardia (pVT), a single defibrillation attempt should be performed on-scene, followed by rapid transport and rewarming:
- CPR and further defibrillation attempts and epinephrine administration should be performed en route:
- This differs from standard treatment for normothermic VF/pVT cardiac arrest
- There is no proven benefit for the administration of amiodarone, lidocaine or other anti-arrhythmics in hypothermic arrest due to VF/pVT
- Patients with Stage IV hypothermia should NOT be considered dead until rewarming has been performed at the appropriate receiving hospital:
- Pre-hospital CPR should be withheld or termination of resuscitation efforts should be considered ONLY if there are obvious signs of irreversible death, there is a valid OOH-DNR order, or conditions are unsafe for EMS Providers
- Refer to the relevant UTSW/BioTel EMS Treatment Guidelines and Policies, especially the ALTERED LEVEL OF CONSCIOUSNESS, ASYSTOLE/PEA, CARDIAC ARREST, POST-CARDIAC ARREST, TRAUMA and VFIB/pulselessVTACH Treatment Guidelines, and the DESTINATION and DETERMINATION of DEATH Policies
- Consult BioTel at any time with questions or concerns
References and Resources:
Appendix – Active Internal and Invasive Rewarming Methods (Refer to Table 2):
- Intravascular Temperature Management
- A special central venous catheter warms the patient by heat exchange, as blood passes over special saline-filled balloons on the catheter in a large vein
- Other methods that can be used in special circumstances, if available:
- Hemodialysis
- Venovenous or Venoarterial ECMO (a form of cardiopulmonary bypass)
- Cardiopulmonary Bypass
- Other methods:
- Infusing warm fluids into the peritoneal or thoracic cavity, stomach or bladder