July 7, 2015
Purpose:
To set forth for UTSW/BioTel EMS Providers current information about the ongoing international outbreak of Middle East Respiratory Syndrome (MERS).
Background:
- MERS is an acute respiratory illness caused by a Coronavirus (MERS-CoV). The virus spreads from ill persons through unprotected close contact with respiratory secretions (e.g. caring for or living with an infected person). It is NOT spread through casual contact.
- Since first reported in 2012, all cases worldwide have been directly or indirectly linked to travel to or residence in countries in the Arabian Peninsula (especially Saudi Arabia); there were 2 cases in the U.S. in 2014. About 35% of patients reported with MERS have died.
- As of June 30, the Republic of Korea (“South Korea”) has confirmed 181 MERS cases, including 33 deaths (the largest known MERS outbreak outside the Arabian Peninsula). Over 13,000 persons have completed quarantine; 8% of cases were healthcare providers.
- This outbreak and ongoing global travel emphasize the continued risk of MERS-CoV spread to the United States, including the Dallas-Fort Worth region.
- EMS providers should be aware of how to identify this disease and how to prepare for its potential arrival.
- The CDC is closely monitoring the situation to better understand this virus.
- New information presented in this EMS Alert may change, as the situation evolves.
Critical Points:
- All EMS Providers shall at all times adhere to all UTSW/BioTel EMS System Guidelines and agency recommendations for Respiratory Hygiene, Cough Etiquette and the prevention of transmission of MERS-CoV and other communicable diseases:
- General infection control guidelines are summarized below.
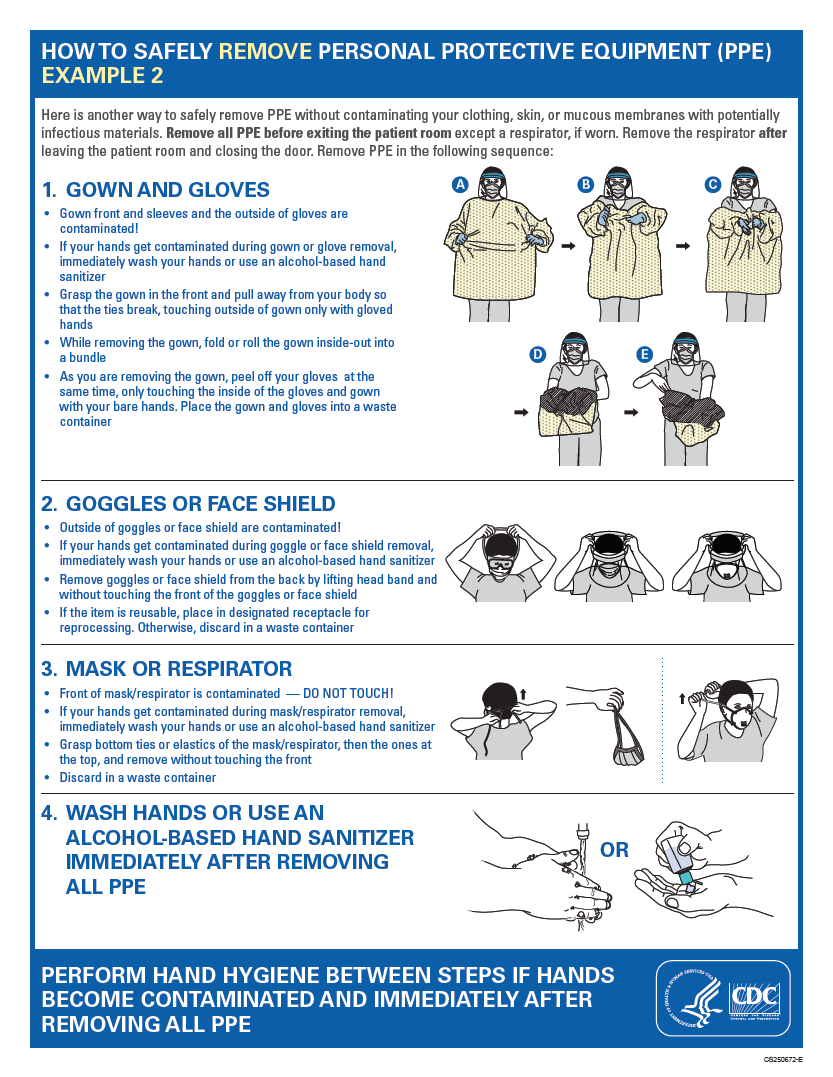
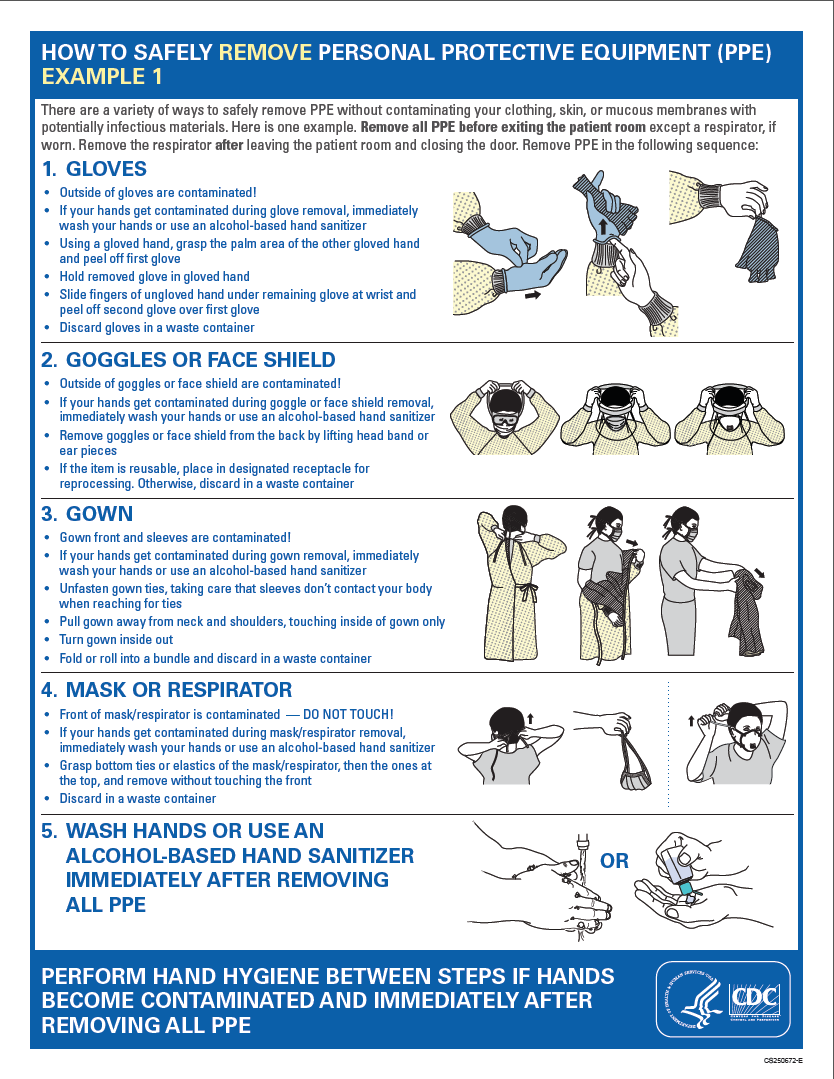
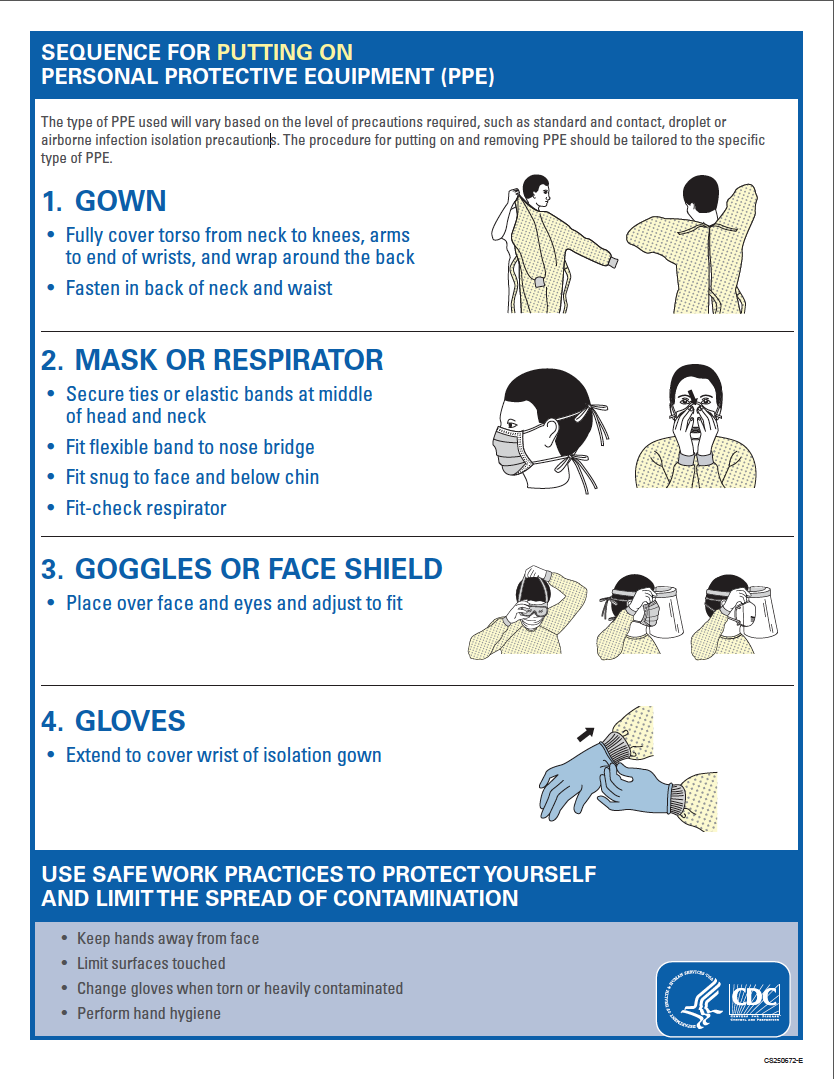
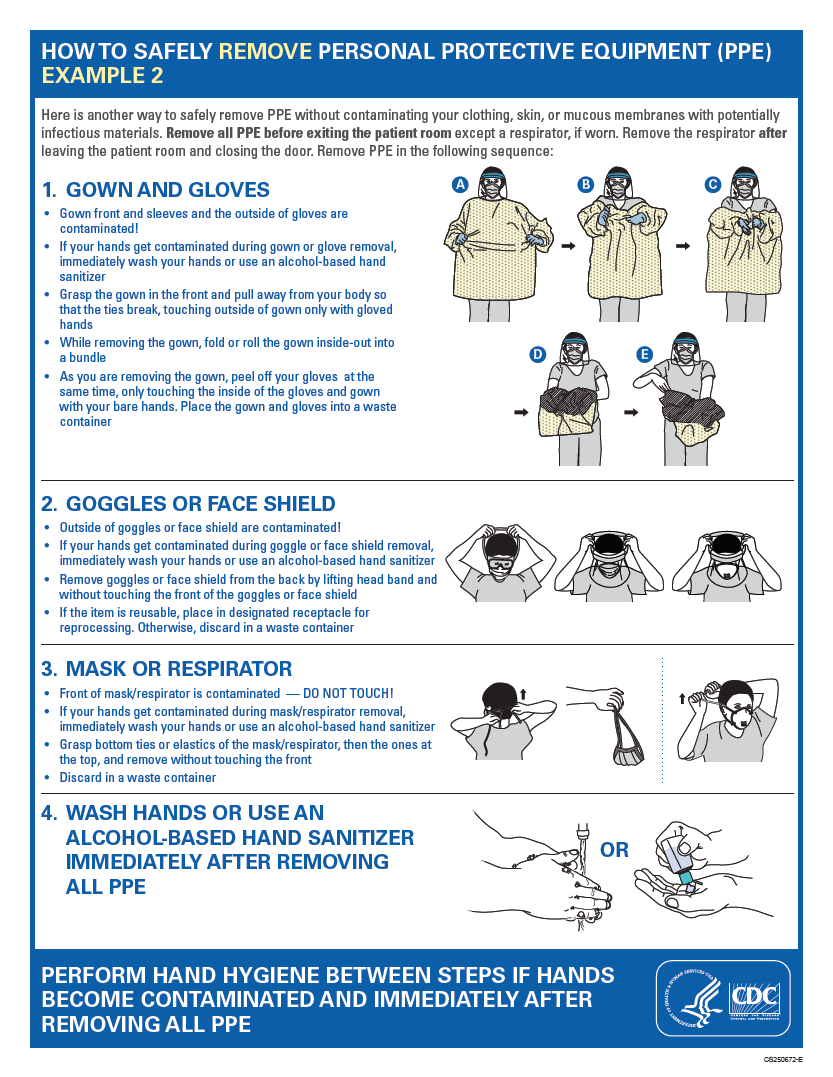
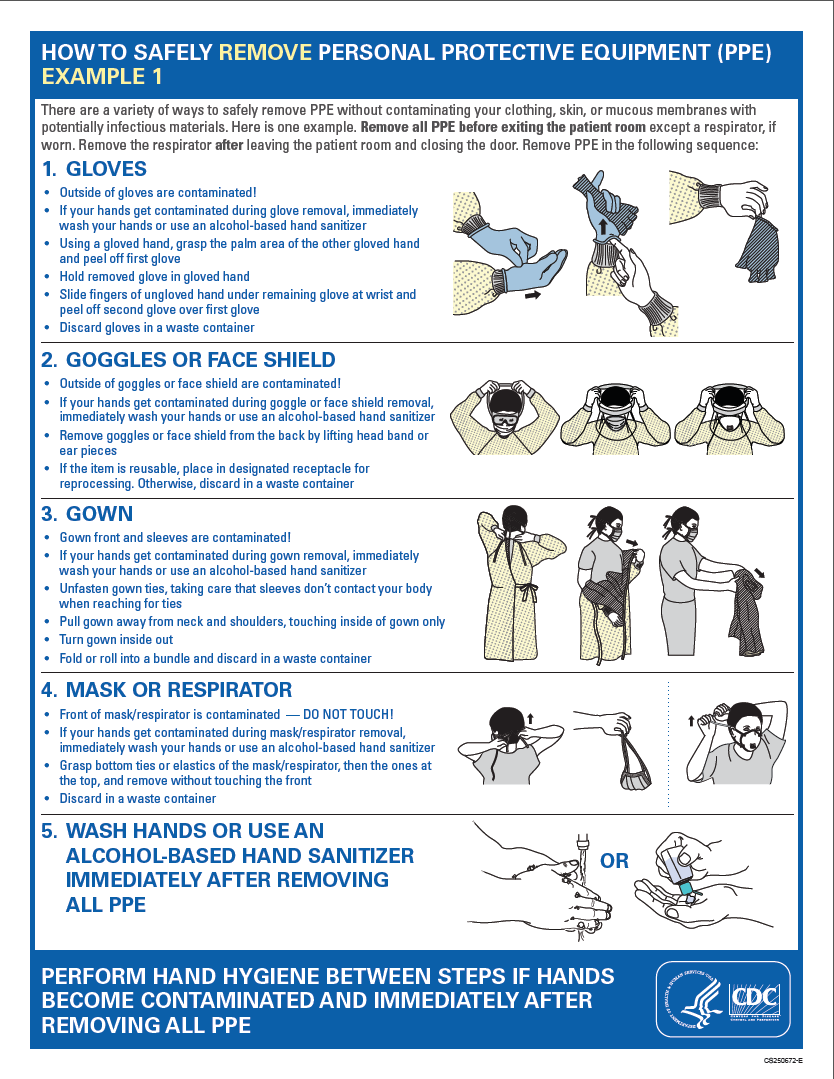
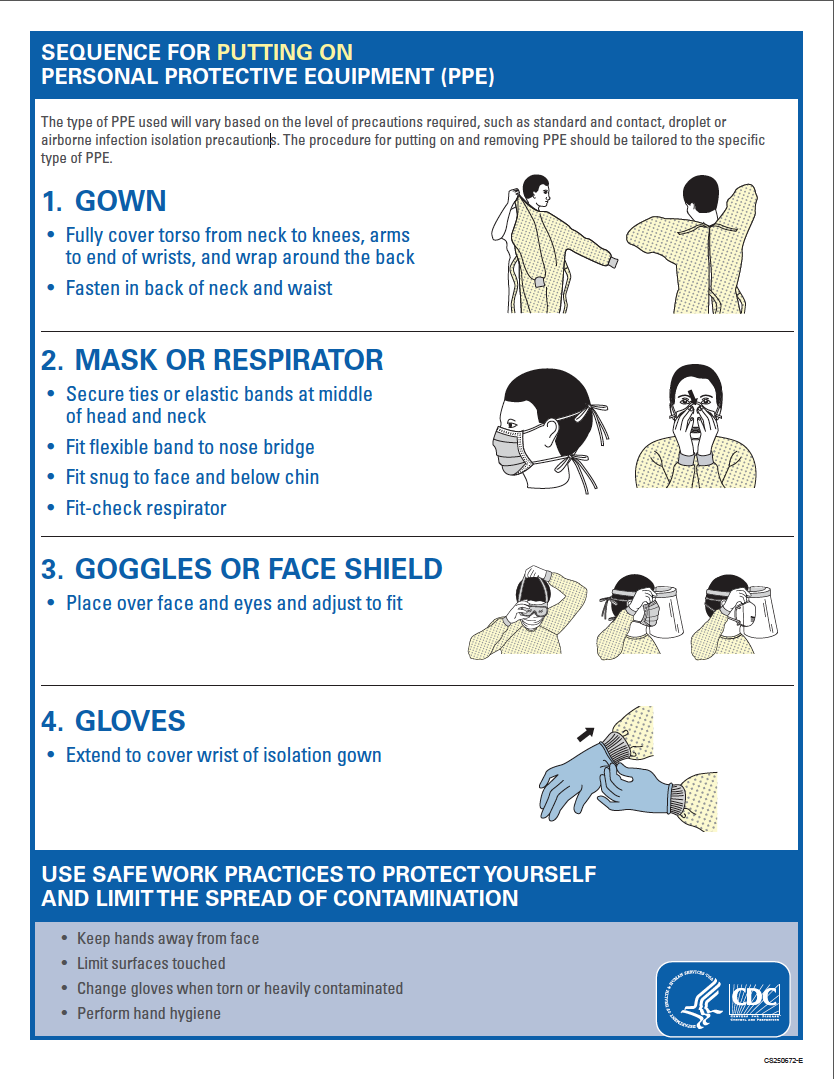
- Specific EMS Infection Control, PPE and Decontamination Guidelines may be found below, and in the CDC PPE Poster (also below and available as a separate downloadable PDF here), and at the CDC web site.
- New guidance will be provided to the UTSW/BioTel EMS System, when available.
- EMS Providers shall continue to routinely ask their patients about their travel history and healthcare facility exposure, and to consider the possibility of MERS-CoV infection in patients meeting criteria (below) for a “Patient Under Investigation” (PUI).
- For any patient meeting criteria as a possible MERS PUI, EMS Providers shall:
- Utilize stringent Standard, Contact and Airborne isolation precautions; and
- Transport the patient to the receiving hospital’s Emergency Department; and
- Notify BioTel AND Emergency Department personnel of the possibility of MERS.
Clinical Presentation (Patient History, Signs, and Symptoms):
- All known cases have been related directly either to the Arabian Peninsula, to travel to that region, or to exposure via close contact with an infected person or in a healthcare facility.
- The incubation period is typically 5 days (range 2 to 14 days).
- Most patients with MERS experience fever, headache, cough and shortness of breath.
- Other symptoms include: sore throat, diarrhea, nausea and vomiting.
- Rapid progression to pneumonia and severe, acute respiratory illness within a week of illness onset can occur, particularly in patients with underlying medical conditions.
Diagnosis and Treatment:
- Diagnostic confirmation requires special tests performed on patient respiratory and blood samples obtained at the hospital and submitted to the Dallas County Health and Human Services (DCHHS) laboratory.
- There is no specific treatment or vaccine for MERS; treatment consists of supportive and symptomatic measures.
CRITICAL EMS SCREENING, TRANSPORT and NOTIFICATION INFORMATION:
- These are the MERS-CoV PUI screening criteria. Patients may fall into one of two groups:
- Fever AND acute respiratory illness symptoms (e.g. cough and shortness of breath) AND ANY of the following:
- History of travel from countries in or near the Arabian Peninsula within 14 days before symptom onset {Includes Bahrain; Iraq; Iran; Israel, West Bank and Gaza; Jordan; Kuwait; Lebanon; Oman; Qatar; Saudi Arabia; United Arab Emirates; Yemen}; OR
- Close contact with a traveler who developed fever and acute respiratory symptoms within 14 days of travel from a country in or near the Arabian Peninsula; OR
- History of being in a healthcare facility (as a patient, worker or visitor) in the Republic of Korea (“South Korea”) within 14 days of symptom onset; OR
- Fever OR respiratory symptoms, AND close contact with a confirmed MERS patient while the patient was ill.
- Any patient meeting PUI screening criteria listed above should be evaluated, transported to a hospital Emergency Department, and reported to BioTel, preferably before hospital arrival. BioTel will inform Dallas County Health and Human Services at 214-677-7899. DCHHS will follow-up with the hospital regarding the outcome of their clinical evaluation.
General Infection Control and Prevention Measures:
- Use rigorous hand hygiene, washing hands before and after EVERY patient contact for at least 20 seconds with soap and water or alcohol-based hand gel.
- Avoid touching eyes, nose and mouth with unwashed hands.
- Avoid close contact (e.g. kissing, hugging, or sharing cups/eating utensils) with persons who are experiencing respiratory symptoms or fever.
- Cover coughs and sneezes with a tissue or shirt sleeve, not your hands. Immediately discard a used tissue in the trash.
- Clean and disinfect frequently-touched surfaces especially in areas where ill persons have come into contact. Examples include: ambulance steering wheel, door handles, stretcher rails, and jumpseat; stethoscope and other medical equipment; and computer keyboards.
- When ill, try to avoid public places and travel, and stay home, if possible.
EMS PPE and Infection Control Measures – These are the same as those used for known or suspected cases of Tuberculosis, measles and other respiratory illnesses:
- Standard, Contact and Airborne Precautions shall be used for contact with all patients with fever, acute respiratory symptoms, and possible MERS-CoV infection (according to PUI screening criteria on p. 2). This includes at least the following items:
- Disposable gown (fluid-impermeable);
- Respiratory protection (N95 respirator);
- Eye protection (disposable face shield or clean reusable goggles);
- Clean non-sterile gloves (double-gloving is not required).
- Implement source-control:
- Standard surgical mask for the patient, if tolerated, until placement in an Airborne Isolation Room is possible;
- For mildly ill patients requiring supplemental oxygen, nasal cannula oxygen, plus a standard surgical mask;
- For severely ill patients, a non-rebreather mask with 100% oxygen or advanced airway management may be needed:
- Special caution should be used during aerosol-generating procedures, such as airway suctioning and advanced airway placement.
- Proper removal (doffing) of PPE – Refer to the CDC PPE Poster below:
- CRITICAL CONCEPT: Do NOT contaminate your clothing, skin, or mucous membranes – especially your eyes, nose or mouth. If hands become contaminated at any step of PPE removal, immediately wash them or use alcohol-based sanitizer.
- Rigorous hand hygiene immediately after removing PPE.
- Standard cleaning and disinfection procedures of ambulance surfaces and equipment, as well as routine management of laundry and medical waste.
SUMMARY:
- There are currently no known, confirmed or suspected MERS cases in the Dallas-Fort Worth area.
- Global travel increases the likelihood of spread of MERS-CoV to this region.
- EMS Providers must remain vigilant, obtain an accurate travel history for all patients, and adhere to stringent infection control and prevention guidelines to protect themselves, their coworkers, other healthcare providers, and their family/loved ones.
Resources (accessed June 29, 2015):
- CDC MERS Index Page
- CDC MERS Healthcare Professionals Information
- CDC Interim Infection Prevention and Control Recommendations for Hospitalized Patients with Middle East Respiratory Syndrome Coronavirus (MERS-CoV)
- CDC MERS Case Definitions
- CDC PPE Sequence Poster – 10/2014
- UTSW/BioTel EMS Guidelines for Therapy
- UTSW/BioTel EMS System Training Bulletin 14-008 Decontamination